Navigating Discomfort
Radiation therapy is a non-invasive and non-painful cancer treatment. However, some patients might experience mild discomfort during treatment sessions, determined by a variety of factors. Physical discomfort due to positioning and immobilisation represent one of the most common causes [1]. Despite the medical team’s efforts, keeping the same position becomes challenging, especially in the case of longer treatment sessions. Most of the external beam radiotherapy (EBRT) sessions last a few minutes, the total time needed expanding up to 15-30 min and rarely up to 1 hour, including patient positioning [2].
Brachytherapy (BT) has the advantage of precise delivery of X-rays in the close proximity of the tumour, being an important technique for treating gynaecological and prostate cancers. For advanced stages of cervical cancer, external and internal irradiation (through BT) are combined for achieving the best results. Unlike the EBRT, where the X ray source is located outside the body, BT requires internal positioning of the ionising radiation sources. Various types of devices placed in the uterus and vagina work as support or as channels for insertion and removal of the radioactive material. The irradiation itself has a length of a few minutes, but the total duration is a result of multiple steps that are aimed to ensure a quality treatment. Due to the increased sensitivity of some anatomical structures, gynaecological brachytherapy requires pain management, sedation, and/or anaesthetic procedures.
Another difference between EBRT and BT workflow is the treatment planning. In the case of EBRT the planning CT scan is followed by contouring and planning, which are usually done during the following days after the scan. When the preparations are ready, the patient comes for the treatment sessions and leaves the department in a short time after each session. In the case of BT the patient enters the department, goes through clinical evaluation, anaesthesia or sedation, then applicator insertion, and then a CT or MRI scan to confirm the correct positioning of the applicator. Contouring and planning is then made with the patient having the applicator in place, which involves an additional time pressure on the medical team to prepare the best quality treatment planning in the shortest possible interval. The current irradiation plan has to take into account the previously received dose by bladder, rectum, sigmoid and small bowel loops during the external beam sessions. The preparation and quality assurance steps, number of BT sessions and their schedule may differ depending on the clinic’s protocols, as well as the total time spent with the applicator in place. A slow process means longer time with the BT applicator in vagina and uterus, patients being under sedation or anaesthesia.
Objective measurements and patients’ feedback
According to a recent survey including data from 39 UK brachytherapy centres, the number of hours with applicators in place per insertion varied from 3 to 53 hours [3]. In the USA, a Stanford team prospectively recorded data from 145 consecutive tandem and ovoid treatments for 33 patients. They found out that the average applicator in place time was 179 minutes (range: 87-311 minutes). Two important factors that increased the duration of having the applicator in treatment position were anaesthesia (additional 42 minutes compared with those who received conscious sedation) and MRI scan after inserting the applicator (additional 66 minutes). Having 3 or more procedures scheduled in the same day led to additional 35 minutes, on average [4].
Beyond the objective evaluations of involved time and resources, patients’ perspective represents a crucial aspect.
A prospective, observational study of 50 patients with locally advanced cervical cancer treated with definitive radio(chemo)therapy with curative intent was carried out by a team from Vienna, coordinated by professor Richard Pötter. They evaluated the incidence and risk factors for post traumatic stress disorder (PTSD) symptoms after High-Dose-Rate (HDR) BT with 2 fractions in 1 application under spinal/epidural anaesthesia. The subjective stress level was rated on a scale from 1 to 10, with 10 points indicating the maximum stress level. BT was rated with a median of 8 points, significantly higher compared with EBRT (median 3), or chemotherapy (median 5). Symptoms of acute stress disorder occurred in 30% of patients 1 week after treatment; and of PTSD in 41% 3 months after treatment in association with this specific BT procedure. Stressful factors were pain, organisational problems during treatment, and immobility between brachytherapy fractions. A table including examples of the most vivid qualitative reports of the brachytherapy experience, using the patients’ own exact wording, is especially touching, because we understand better how patients perceive the procedure [5].
Another study, this time from the UK, used semi structured interviews with 35 patients from 4 clinics who had received BT for locally advanced cervical cancer – either recently had BT, either 2 years before the interviews. Consecutive patients from 4 clinics were included. Insertion and removal of applicators, duration of applicators being inside them, lying flat for a long time, and side effects created unpleasantness and discomfort. Difficult and traumatic experiences were reported, including periods of severe pain and perceptions of poor care [6].
Possible ways of improvement
Irrespective of the protocol and type of BT, it is reasonable to consider that a decrease in treatment preparation time would be beneficial for the patient and the medical team.
The MRI-guided BT has the advantage of better target visualisation and treatment adaptation, being recommended by professional societies, internationally [7-9]. As a result, avoiding MRI to reduce treatment time is not a logical option.
Pain and discomfort represent limiting factors of gynaecological BT, sometimes leading to unsatisfactory results in terms of adequate position of the applicator set. Local anaesthesia is recommended for procedures shorter than 30 min and some techniques would not offer effective pain relief. Conscious sedation is less complex compared to anaesthesia, offers a faster recovery and it is recommended whenever possible by the American Society of Brachytherapy. However, there are reports on a series of patients in which the majority acknowledged mild to moderate pain despite conscious sedation. As a result, avoiding anaesthesia with the aim of decreasing treatment duration is not an ethical choice [10].
Using the same plan for multiple sessions in order to save time is not an optimal solution, either. A dosimetric analysis of using a single treatment plan for multiple treatment fractions in gynecologic brachytherapy was made by a team of professionals from University of California San Francisco. They concluded that when the Day 1 plan was used on the Day 2, the HR-CTV coverage decreased significantly (p < 0.0001). Despite the short interval between fractions, the rectum V75 significantly increased, there were volume changes in the HR-CTV contour, and the maximum applicator and catheter displacements ranged from 10 to 30mm [11].
A team from Dana Farber Cancer Institute tried to identify all tasks and associated resources involved in cervical cancer brachytherapy, arrange them in a process map and redesign the treatment planning component to minimise planning time [12]. Apart from this type of workflow-level intervention, improvements of separate components of the process can be efficient. A prospective evaluation of an in-house automatic contouring model developed by an Alabama team showed statistically significant time reduction for contour approval time and total planning time in the prospective auto-contoured cohort compared to retrospective manually contoured cohort [13].
Our solution
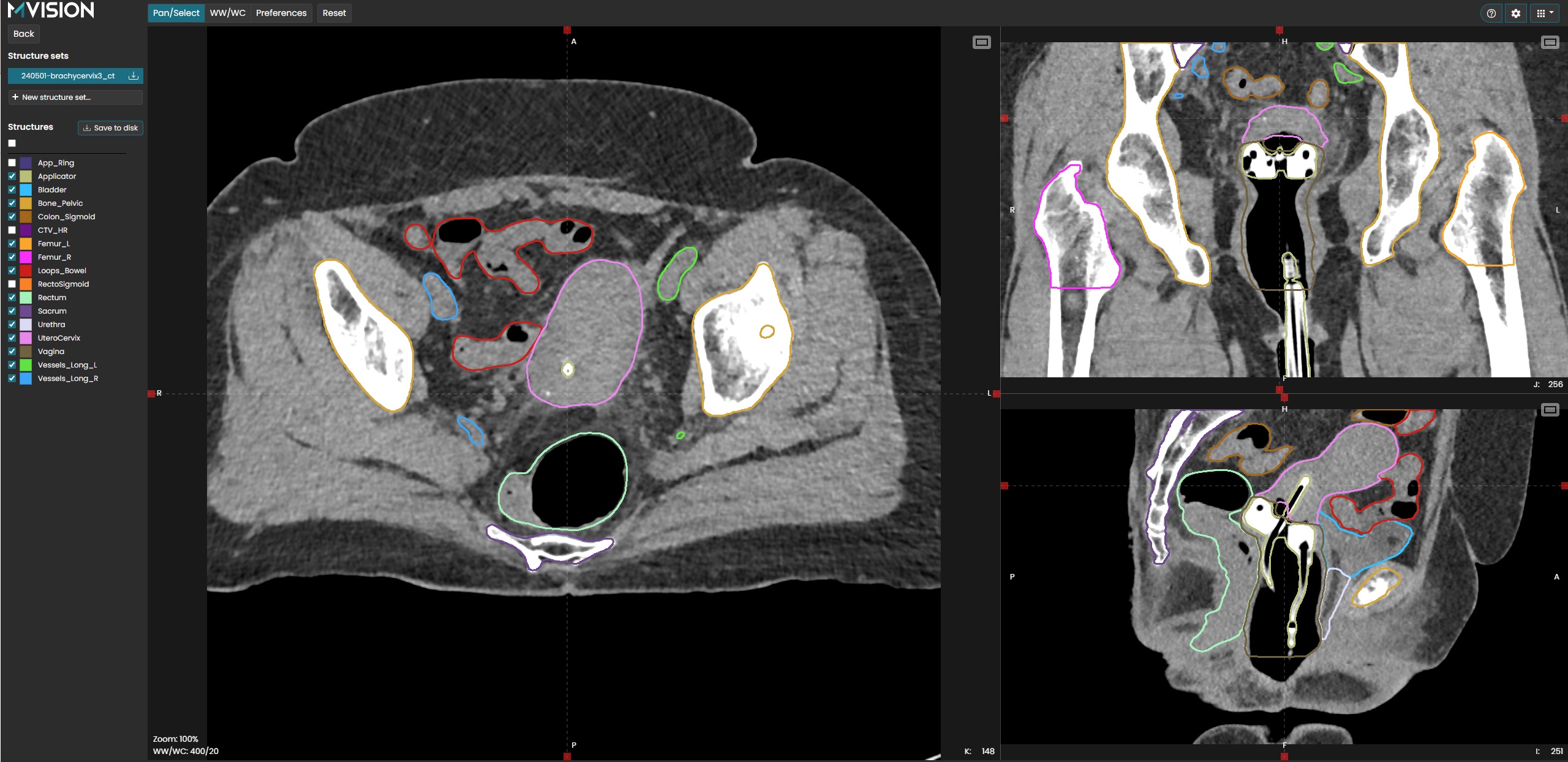
One of MVision’s core values is contributing to offering the best possible cancer care. The new version of MVision AI Contour+ solution offers the CT cervix brachytherapy model, which provides 15 regions of interest. Except for the frequently used organs at risk, such as bladder, rectum sigmoid colon and bowel loops, the model accurately predicts the urethra, vagina and utero-cervix and pelvic vessels. Femoral heads, sacrum and pelvic bones are also part of the structures’ list. Additionally, the vaginal applicator and applicator’s ring are recognized and delineated. The structures that were used to train the model were following international guidelines such as RTOG 2012 (Gay et al), GHG 2020 (Mir et al), 2020 GEC-ESTRO (Schmid et al.), PIVOTAL 2015 (Harris et al). When a clear description of an anatomical structure in an international contouring guideline was not found, Gray’s anatomy was used as a reference.
References
- Goldsworthy, S.D., Tuke, K., & Latour, J.M. (2016). A focus group consultation round exploring patient experiences of comfort during radiotherapy for head and neck cancer. Journal of Radiotherapy in Practice, 15, 143 – 149.
- https://www.cancer.org/cancer/managing-cancer/treatment-types/radiation/external-beam-radiation-therapy.html
- Humphrey, P., Dures, E., Hoskin, P.J., & Cramp, F. (2020). A UK survey of brachytherapy practice for locally advanced cervical cancer. Radiography, 26.
- Usoz M, von Eyben R, Fujimoto DK, Kidd EA. Improving gynecologic brachytherapy patient experience by optimizing MRI, anesthesia, and scheduling to decrease the length of time tandem and ovoid applicators are in place. Brachytherapy. 2020;19(2):162-167. doi:10.1016/j.brachy.2019.11.011
- Kirchheiner, K., Czajka-Pepl, A., Ponocny-Seliger, E., Scharbert, G., Wetzel, L., Nout, R. A., Sturdza, A., Dimopoulos, J. C., Dörr, W., & Pötter, R. (2014). Posttraumatic stress disorder after high-dose-rate brachytherapy for cervical cancer with 2 fractions in 1 application under spinal/epidural anesthesia: incidence and risk factors. International journal of radiation oncology, biology, physics, 89(2), 260–267.
- Humphrey P, Dures E, Hoskin P, Cramp F. Patient Experiences of Brachytherapy for Locally Advanced Cervical Cancer: Hearing the Patient Voice Through Qualitative Interviews. Int J Radiat Oncol Biol Phys. 2024;119(3):902-911. doi:10.1016/j.ijrobp.2023.12.016
- Mahantshetty U, Poetter R, Beriwal S, et al. IBS-GEC ESTRO-ABS recommendations for CT based contouring in image guided adaptive brachytherapy for cervical cancer. Radiother Oncol. 2021;160:273-284. doi:10.1016/j.radonc.2021.05.010
- ASTRO Guideline on Radiation Therapy for Cervical Cancer, accessed on 31 August 2024, available at https://www.astro.org/patient-care-and-research/clinical-practice-statements/cervical-cancer-guideline
- Dimopoulos JC, Petrow P, Tanderup K, et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (IV): Basic principles and parameters for MR imaging within the frame of image based adaptive cervix cancer brachytherapy. Radiother Oncol. 2012;103(1):113-122. doi:10.1016/j.radonc.2011.12.024
- Pellizzon ACA. Pain relief procedures before high-dose-rate brachytherapy for non-surgical treatment of cervix cancer. J Contemp Brachytherapy. 2018;10(6):567-569. doi:10.5114/jcb.2018.81027
- Pinnaduwage DS, Cunha JA, Weinberg V, et al. A dosimetric evaluation of using a single treatment plan for multiple treatment fractions within a given applicator insertion in gynecologic brachytherapy. Brachytherapy. 2013;12(5):487-494. doi:10.1016/j.brachy.2013.02.003
- Damato AL, Lee LJ, Bhagwat MS, et al. Redesign of process map to increase efficiency: Reducing procedure time in cervical cancer brachytherapy. Brachytherapy. 2015;14(4):471-480. doi:10.1016/j.brachy.2014.11.016
- Kraus AC, Iqbal Z, Cardan RA, et al. Prospective Evaluation of Automated Contouring for CT-Based Brachytherapy for Gynecologic Malignancies. Adv Radiat Oncol. 2023;9(4):101417. Published 2023 Dec 10. doi:10.1016/j.adro.2023.101417