The multi-step radiation therapy process involves coordination of different devices and systems. Starting with electronic health records where clinical data are stored, and continuing with CT simulation, contouring, planning and treatment delivery, data transfer and harmonization still require significant manual input.
Using a platform that integrates multiple facilities, such as a workspace platform, has multiple advantages. Separate solutions can perform reasonably well, but manually synchronizing their inputs and outputs can bring additional challenges.
Below, we discuss the reasons for implementing an integrated workspace in radiation oncology and highlight practical considerations.
1. Rationale for using integrated platforms
1.1 The psychological perspective
Human cognition is limited in working memory and attention span. Constantly switching between tools forces users to re-orient repeatedly, increasing mental fatigue. Frequent interruptions decrease performance and increase the likelihood of errors. This hypothesis has been confirmed by studies on different subjects, such as web developers, emergency doctors and nurses (1-3).
Interestingly, digital integration seems to foster psychological empowerment. Employees feel more competent, autonomous, and satisfied when systems are coherent and reduce frustration from tool fragmentation. Improved self-efficacy correlates with greater technology acceptance and job satisfaction (4).
Integrated systems reduce interruptions tied to switching tools, logging into separate apps, or synchronizing separate datasets. As a result, unified platforms enable users to stay in a stable mental context and preserve cognitive resources for higher-level tasks (planning, quality checks, clinical reasoning). This effect is particularly important for demanding environments such as radiation oncology, where workflow clarity and predictable tools reduce anxiety and support sustained attention.
Moreover, integrated platforms support shared mental models. Common data views and workflows encourage teams to form a unified understanding of task states, which leads to better coordination and fewer miscommunications.
1.2 The operational perspective
Data silos arise when data is isolated across multiple systems that do not readily communicate with one another, preventing the formation of a comprehensive, shared data view and hindering collaborative workflows. Integrated platforms eliminate this challenge, reducing time wasted on manual reconciliation, by providing a single version of truth. Therefore, the decision-making process becomes more efficient (5)
Integrated solutions lead to lower operational costs, fewer errors, better collaboration, and streamlined IT management (6).

2. Applications in technology and healthcare
2.1 Integrated toolchains in software engineering
Continuous integration represents a software engineering technique that uses automation to integrate small, frequent code updates. A systematic review of published literature on this topic which included 101 studies, showed that integrating build, testing, and deployment processes into a unified pipeline results in faster feedback loops, better team collaboration and consistent quality assurance, when compared to fragmented toolchains requiring manual coordination. Radiation Oncology is a medical field where technology plays a vital role, so it makes perfect sense to apply the same principles for Radiotherapy-dedicated solutions (7).
2.2 Advantages of integrated tools in healthcare
A scoping review of electronic health record interoperability highlighted the benefits of integrating disparate health systems. It described semantic and technical interoperability as critical factors for efficient data exchange, improved decision quality and clinical coordination. Integrated systems support unified data access, helping clinicians work with complete patient information rather than fragmented data (8).
A perspective article on digital information ecosystems, published in the Journal of Medical Internet Research, shows that integration of clinical tools significantly enhances care coordination, reduces communication gaps across the care pathway, and mitigates clinician workload tied to fragmented systems (9).
3. Special considerations for radiation therapy
3.1 Enhanced workflow efficiency and speed
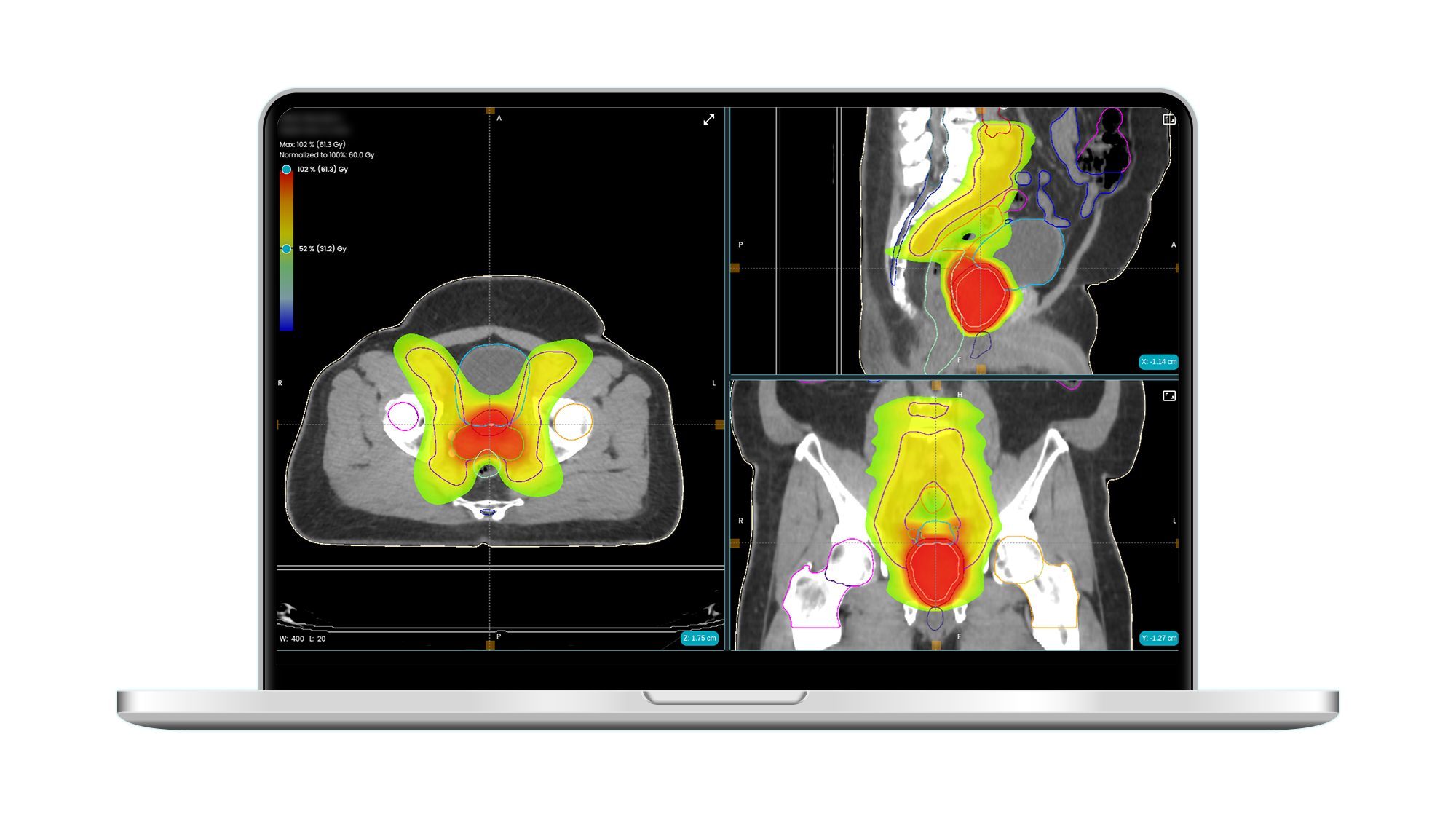
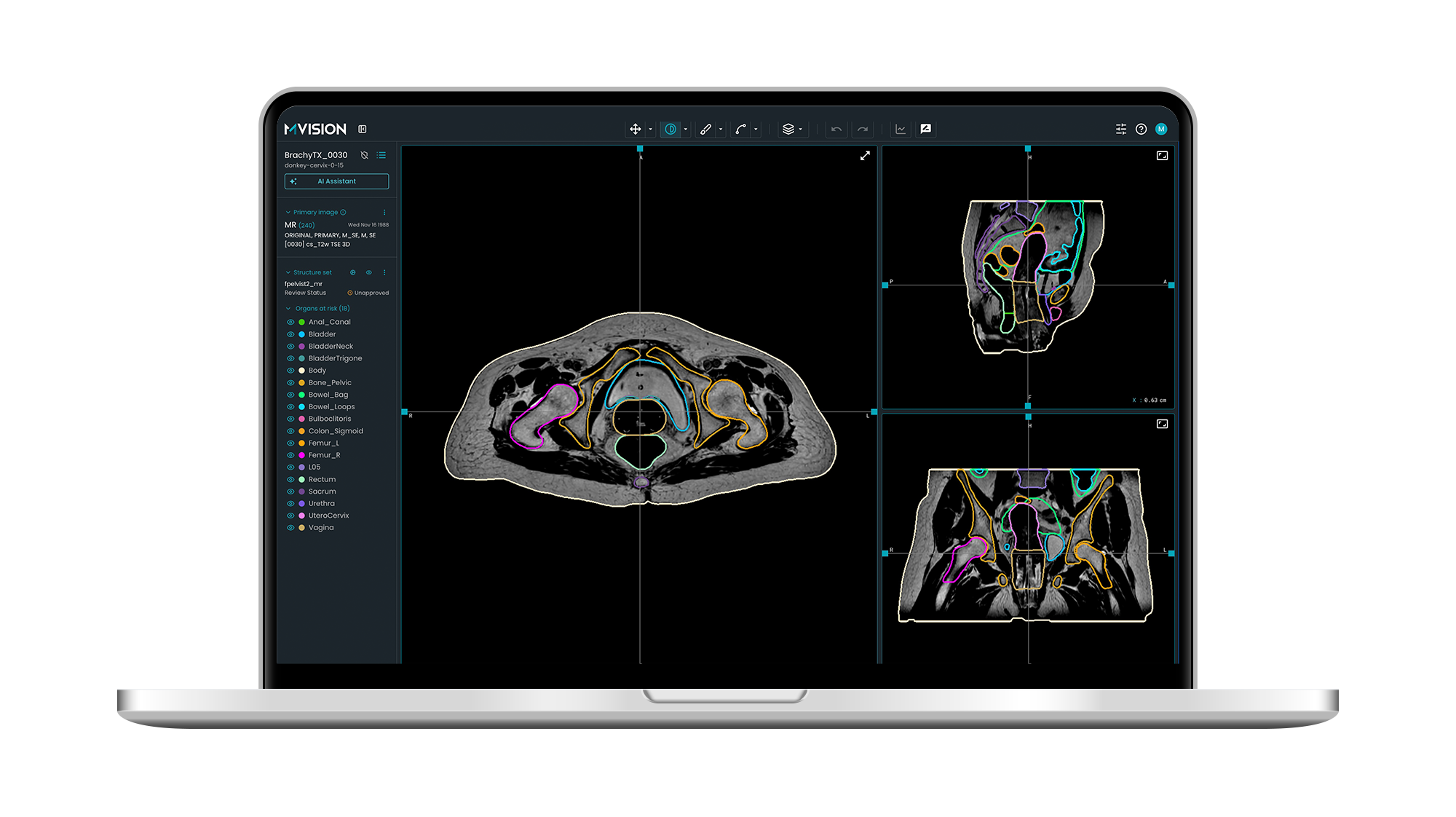
Integrated platforms enable seamless transitions between simulation, contouring, planning, image guidance, and delivery. A technical note published in Medical Physics presented a CT-integrated linear accelerator and AI model implementation. The fully automated “All-in-One” radiotherapy workflow was evaluated for ten rectal cancer patients. The entire process—including simulation, autosegmentation, autoplanning, image guidance, beam delivery, and in vivo quality assurance—was completed in 23.2 ± 3.5 minutes while the patient remained on the treatment couch (10).
3.2 Improved treatment quality and consistency
Centralized platforms facilitate standardized protocols, automated contouring, and planning, which reduce inter-operator variability and errors. The automated plans created by a software developed in-house were compared with manual plans for 56 patients treated with intensity modulated radiation therapy. The automated plans reduced the average optimization time by 77.3% and significantly reduced the doses for the spinal cord, esophagus, heart, aorta and main bronchus. Radiation Oncologists considered more than 75% of the automated plans acceptable without corrections (11).
3.3 Real-time adaptive planning and quality assurance
Integrated imaging and automation support online adaptive replanning and in vivo QA, ensuring accurate dose delivery and the ability to respond to anatomical changes during treatment. A study that evaluated the ART2Dose, a secondary dose verification software reported reduced time to complete pre-treatment checks by 3-4 min for each plan with gamma passing rates higher than 97% (12).
3.4 Remote collaboration and standardization
Cloud-based and web-based workspace platforms allow remote consultation, plan review, and decision support, enabling under-resourced or community centers to access expert input and advanced planning tools. This leads to improved plan quality, reduced travel time for consultants, and better quality control across multiple sites (13).
Another advantage is represented by enabling harmonization of treatment protocols and benchmarking, which improves compliance and overall treatment quality in multicenter clinical trials and routine practice (14).
4. Summary
Integrated AI platforms in healthcare workflows cut down tool switching, reduce staff frustration, and accelerate care delivery compared with isolated AI tools requiring manual linkage. Radiotherapy platforms where treatment planning, imaging, and quality assurance workflows benefit from reduced tool jumping and unified data models offer:
- Cognitive efficiency: clinicians spend less effort jumping across tools, reducing burnout and increasing clinical time.
- Workflow coherence: unified planning, QA, and delivery modules reduce manual data transfer.
- Error reduction: shared patient models and dosimetry data reduce risks from inconsistent records.
- Improved collaboration: multidisciplinary teams (physicists, therapists, clinicians) share consistent data views.
These advantages collectively result in more precise, efficient, and equitable radiotherapy care, with demonstrable improvements in workflow, plan quality, and patient access.
References
- Zahra Shakeri Hossein Abad, Mohammad Noaeen, Didar Zowghi, Behrouz H. Far, and Ken Barker. 2018. Two Sides of the Same Coin: Software Developers’ Perceptions of Task Switching and Task Interruption. In Proceedings of the 22nd International Conference on Evaluation and Assessment in Software Engineering 2018 (EASE ’18). Association for Computing Machinery, New York, NY, USA, 175–180. https://doi.org/10.1145/3210459.3214170
- Westbrook JI, Raban MZ, Walter SR, et al. Task errors by emergency physicians are associated with interruptions, multitasking, fatigue and working memory capacity: a prospective, direct observation studyBMJ Quality & Safety 2018;27:655-663.
- Westbrook JI, Woods A, Rob MI, Dunsmuir WTM, Day RO. Association of Interruptions With an Increased Risk and Severity of Medication Administration Errors. Arch Intern Med. 2010;170(8):683–690. doi:10.1001/archinternmed.2010.65
- Liu, J., Soomro, H.J. Technology meets psychology: digital finance integration, empowerment, and satisfaction among fintech employees. BMC Psychol 13, 762 (2025). https://doi.org/10.1186/s40359-025-03104-1
- https://www.delphialliance.com/post/benefits-of-one-integrated-software-solution-with-multiple-modules-vs-multiple-standalone-solutions
- https://www.simbo.ai/blog/benefits-of-integrated-ai-platforms-over-isolated-ai-solutions-in-healthcare-for-seamless-workflow-integration-and-scalable-clinical-collaboration-3781230/
- Soares, E., Sizilio, G., Santos, J., Da Costa, D. A., & Kulesza, U. (2022). The effects of continuous integration on software development: a systematic literature review. Empirical Software Engineering, 27(3), 78.
- Zhang X, Saltman R. Impact of Electronic Health Record Interoperability on Telehealth Service Outcomes. JMIR Med Inform. 2022;10(1):e31837. Published 2022 Jan 11. doi:10.2196/31837
- Chen Y, Lehmann CU, Malin B. Digital Information Ecosystems in Modern Care Coordination and Patient Care Pathways and the Challenges and Opportunities for AI Solutions. J Med Internet Res 2024;26:e60258. doi: 10.2196/60258
- Yu L, Zhao J, Xia F, et al. Technical note: First implementation of a one-stop solution of radiotherapy with full-workflow automation based on CT-linac combination. Med Phys. 2023;50(5):3117-3126. doi:10.1002/mp.16324
- Vanderstraeten B, Goddeeris B, Vandecasteele K, van Eijkeren M, De Wagter C, Lievens Y. Automated Instead of Manual Treatment Planning? A Plan Comparison Based on Dose-Volume Statistics and Clinical Preference. Int J Radiat Oncol Biol Phys. 2018;102(2):443-450. doi:10.1016/j.ijrobp.2018.05.063
- Lin J, Chen M, Lai Y, et al. ART2Dose: A comprehensive dose verification platform for online adaptive radiotherapy. Med Phys. 2024;51(1):18-30. doi:10.1002/mp.16806
- Zhou Y, Luo B, Sang J, et al. A cloud-based consultation and collaboration system for radiotherapy: Remote decision support services for community radiotherapy centers. Comput Methods Programs Biomed. 2023;229:107270. doi:10.1016/j.cmpb.2022.107270
- Giglioli FR, Garibaldi C, Blanck O, et al. Dosimetric Multicenter Planning Comparison Studies for Stereotactic Body Radiation Therapy: Methodology and Future Perspectives. Int J Radiat Oncol Biol Phys. 2020;106(2):403-412. doi:10.1016/j.ijrobp.2019.10.041














