Across much of the world, men are living into older age in greater numbers than ever before. With this increase in years comes a different pattern of illness, one in which prostate cancer plays a leading role. Prostate cancer cases are climbing, driven not only by longer life expectancy, but also by population growth and increased detection through prostate-specific antigen (PSA) testing.
As cases rise, the demand for more precise and accessible treatment is growing, with prostate cancer radiotherapy planning playing an ever more critical role.
Prostate cancer is now the most commonly diagnosed cancer (excluding non-melanoma skin cancers) in men across more than 110 countries. Its global impact is set to grow dramatically. The Lancet Commission on Prostate Cancer projects that annual new cases will more than double from 1.4 million in 2020 to nearly 3 million by 2040. The commission also predicts that deaths will rise by almost 85% over the same period (1).
Although prostate cancer occurs worldwide, trends vary between regions. In higher-income countries, advanced screening, imaging, and treatment have helped keep death rates steady, even as clinicians diagnose more men. In many low- and middle-income countries (LMICs), however, both incidence and mortality are rising sharply. This is largely due to limited access to early detection tools such as PSA testing, shortages of imaging and pathology services, and a lack of modern treatment infrastructure, including radiotherapy equipment and technology (1).
Prostate cancer cases in 2020
Projected new cases in 2040
Treating Prostate Cancer
Treatment choices for prostate cancer depend on the stage of disease, risk classification, and individual patient factors.
For advanced or metastatic disease, androgen deprivation therapy (ADT) remains the cornerstone of care, often combined with newer androgen receptor pathway inhibitors, and in some cases, chemotherapy. When prostate cancer is localized, physicians may recommend radical prostatectomy (surgical removal of the prostate) to patients who are in good overall health and expected to tolerate surgery well. Radiotherapy is a non-surgical, organ-sparing alternative, frequently used in both localized and locally advanced settings (2).
Each treatment comes with its own side effect profile. Surgery carries higher risks of urinary incontinence and erectile dysfunction, while radiotherapy may also cause erectile dysfunction and urinary symptoms, alongside different degrees of bowel irritation. Treatment selection involves weighing the potential for long-term cancer control against the risks of side effects, the patient’s life expectancy, and their individual values and priorities (2).
Radiotherapy’s Expanding Role
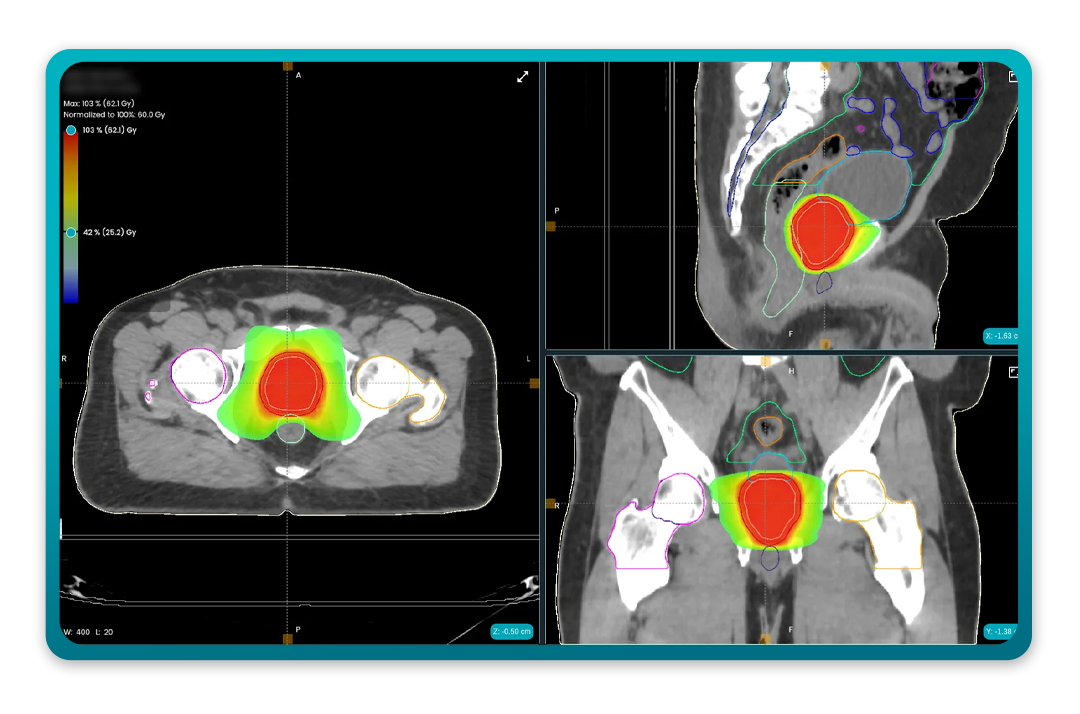
Radiotherapy for prostate cancer has evolved considerably over the last two decades. Advances in imaging, planning, and delivery have improved precision, allowing higher doses to the tumour while better protecting nearby structures such as the bladder, rectum, and neurovascular bundles (2).
Today, radiation oncologists can deliver radiation in several ways, ranging from external beams directed at the prostate (External Beam Radiotherapy, EBRT), to short-course high-dose treatments (Stereotactic Body Radiotherapy, SBRT), to internal radiation delivered through implanted sources (Brachytherapy). Strong clinical evidence supports each method, and clinicians choose among them based on a patient’s disease stage and risk profile (2).
Precision also depends on the accuracy of the treatment plan—defining exactly where the radiation should go and how it should be delivered. This is where AI in prostate cancer radiotherapy planning is beginning to play a transformative role.
Planning Challenges and the Case for AI
Treatment planning for prostate radiotherapy involves key steps, each with room for variation. Clinicians must first contour the prostate, seminal vesicles, and nearby organs-at-risk (OARs) on patient scans. Even among experienced specialists, these contours can differ, which may affect how much radiation the tumour and healthy tissues receive — influencing both cancer control and side effects (2).
Next, clinicians set dose targets for the tumour and limits for surrounding organs. These goals can also vary between planners and are influenced by anatomy, patient positioning, and daily changes such as bladder or rectal filling. Cases involving pelvic lymph nodes add another layer of complexity (2).
Artificial intelligence can help standardise and speed up these steps without removing clinician oversight. By providing high-quality starting points—such as guideline-compliant contours, predicted dose distributions, diagnostic insights, and even support in generating full treatment plans—AI reduces repetitive manual work. This support enables clinicians to spend more time refining strategies and making treatment decisions, while maintaining full control over the process..
Applying AI to Radiotherapy Planning
Across oncology, researchers and technology companies are developing new AI tools to help clinicians spend less time on repetitive planning tasks and more time focusing on patients. The goal is not to replace expertise but to improve accuracy, reduce variation, and make advanced radiotherapy more widely accessible.
MVision AI is one example of this work. Its auto-contouring software, Contour+, can delineate over 300 anatomical structures following internationally recognised guidelines such as RTOG and ESTRO. For prostate cancer, the male pelvis model produces high-accuracy contours for the prostate, seminal vesicles, bladder, rectum, and pelvic lymph nodes. This has been shown to cut manual contouring time by up to 95% while also improving consistency between clinics.
Dose+, another MVision AI tool, uses machine learning to predict achievable 3D dose distributions based on a patient’s CT scan and contours. These predictions can be imported into any DICOM-compliant planning system, providing planners with a strong starting point for optimisation. This is particularly useful in complex cases involving pelvic lymph nodes, where balancing tumour coverage with protection of surrounding organs can require multiple planning iterations.
A case study from the Northern Centre for Cancer Care (NCCC) in Newcastle, UK, evaluated Dose+ in 60 prostate cancer patients—half with prostate-only treatment, half with additional pelvic lymph node irradiation. The study found strong agreement between Dose+ predictions and established automated plans in standard cases. For complex cases, Dose+ helped identify situations requiring early trade-offs between target coverage and organ protection, reducing trial-and-error and saving planning time.
The Future of Prostate Cancer Radiotherapy Planning
AI integration into prostate cancer radiotherapy planning is accelerating. Increasing numbers of clinics now use AI tools for automated contouring and dose prediction in routine workflows, and vendors are embedding these capabilities directly into treatment planning systems. There is also growing interest in genomics-driven radiotherapy, where tumour biology guides not only systemic therapy but also radiotherapy dose and fractionation. AI could be pivotal in merging these biological insights with imaging and planning data (2).
For health systems under strain, particularly in LMICs, AI may help bridge gaps in expertise and capacity. By reducing planning variability and speeding up workflows, AI tools could help more patients access high-quality treatment sooner (1).
References
- James ND, Tannock I, N’Dow J, Feng F, Gillessen S, Ali SA, et al. The Lancet Commission on prostate cancer: planning for the surge in cases. The Lancet. Published online April 4, 2024. https://doi.org/10.1016/S0140-6736(24)00651-2
- National Cancer Institute. Prostate Cancer Treatment (PDQ®)–Health Professional Version. Updated June 27, 2024. https://www.cancer.gov/types/prostate/hp/prostate-treatment-pdq
- American Cancer Society. Key Statistics for Prostate Cancer. Updated January 5, 2025. https://www.cancer.org/cancer/types/prostate-cancer/about/key-statistics.html

