”Our future is a race between the growing power of technology and the wisdom with which we use it.” This statement of Stephen Hawking, the well known physicist, mathematician and visionary, summarizes very well the present challenges. A new technology, irrespective of its degree of complexity, makes an impact in our world depending on the way it is used. More powerful it is, the bigger the impact of using it the right way. Following this judgment, we gathered below some ideas, controversies and news on the ethical use of AI in Radiation Oncology.
Strengths and weaknesses of AI-enhanced healthcare
AI implementation in healthcare opens a wide range of opportunities, from early diagnosis to treatment and follow-up. It can be used as a decision support tool, increasing precision and personalization. Analyzing large amounts of data, identifying patterns and anomalies, predicting outcomes or selecting the best options to be explored further in new drug discovery are only a few of AI applications in medicine. Telemedicine and remote monitoring can improve the quality of care through surveillance for chronic diseases for patients residing far from medical centers, and not only. The AI-based solutions increase efficiency by automating repetitive tasks or creating complex algorithms that are suggesting new ways of reorganizing processes and sparing resources.
However, some aspects of AI use need to be evaluated from an ethical perspective:
- Data privacy and safety – Collecting, storing and processing patients’ data brings new technical challenges and security risks, which leads to new solutions.
- Bias and fairness – Algorithms’ performance is reflecting the training data’s features, which might not be representative for another group or population. Therefore, this aspect needs to be taken into account by industry and the users. Applying a solution for a different purpose that it has been designed for, would not be fair to the patient. Interestingly, a bias can occur also while evaluating the AI-based solutions. Their excellent performance can lead to an overreliance on them. As a consequence, clinicians have to stay alert and well trained, so they can identify possible errors
- Lack of human judgment and empathy – Medical decisions are made by applying a weighted judgment, taking into account multiple aspects, evaluating the context and thinking outside the box. Emotions are part of the connection established between patients and caregivers and are needed for communication, especially on sensitive topics. The absence of complex human interaction can decrease patients’ satisfaction or compliance with treatment. Legal aspects can become important, too. If an error would occur due to a solution suggested by an AI tool, it is debatable who should take responsibility for it.
- Initial Investment and job displacement – Even if in the long term the AI would bring financial benefits, implementing new solutions need to compete in the short term with other expenses. Changing workflows have the potential of changing roles and needs on the workforce market, so before a balance is set, some challenges might appear (1).
AI in Radiation Oncology
AI supports the complex process of individualizing radiotherapy in all its stages: decision, planning and delivery. Moreover, research represents another fertile ground for AI.
- Decision to give radiotherapy is influenced by image features analysis and patient selection criteria, which can benefit from AI-based support tools. Prediction models can be also developed to estimate the risk of treatment side effects and adjust the treatment parameters according to this probability.
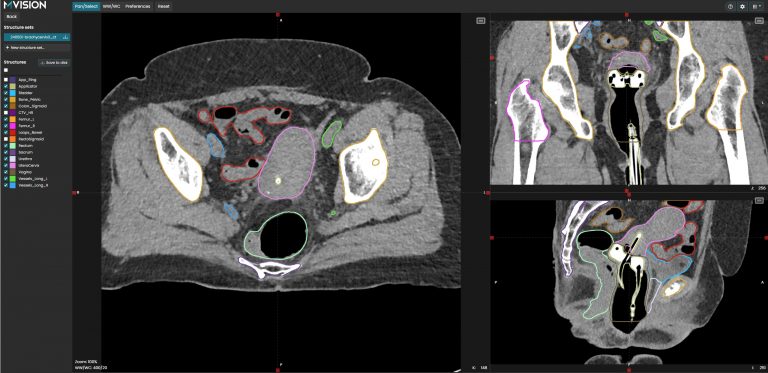
- Planning is highly influenced by AI-based auto-contouring and automatic plan generation. Adaptive radiotherapy is a new field in which automation is needed to speed up the process and increase the quality.
- Delivery is optimized with the help of the AI by smarter treatment scheduling, automatic monitoring during irradiation and optimizing the complex aspects of quality assurance.
- Research integrates AI in data analysis, including image features, like in radiomics studies, and is also providing efficient tools for education. Patients’ follow-up can also benefit from AI-based systems’ capabilities.
General ethical principles like beneficence, non-maleficence, fairness, and respect for autonomy are still valid when integrating AI in radiotherapy. One of the possible pitfalls of AI-offered solutions is that its recommendations can be based on correlations, which do not necessarily imply causality. Human supervision is still needed in order to choose the most appropriate solution. However, the ability to evaluate the validity of automatic solutions requires solid knowledge and sharp skills, which are the result of high quality education.
Since AI-based solutions become available, but they are still not available everywhere, another ethical issue can arise for the clinicians – Should they or should they not inform and eventually redirect the patients in a clinic that has such facilities, if the patients prefer so? This doubt is also related to patients’ perspective, who could either be enthusiastic about AI and overconfident, or, by contrast, reluctant. A balanced, realistic perception of patients (and caregivers, as well) can be created by accurate information regarding AI-based solutions’ performance and limitations (2).
Official recommendations at international level
New solutions bring the need for guidance and regulations. A general guidance document was issued in 2021 by the WHO, identifying six core principles: protect autonomy; promote human well-being, human safety, and the public interest; ensure transparency, explainability, and intelligibility; foster responsibility and accountability; ensure inclusiveness and equity; and promote AI that is responsive and sustainable (3).
The EU AI act, recently issued by the European Parliament, includes the AI systems used in medical devices in the high risk category (4). Other global initiatives, such as the G7 leaders’ agreement on guiding principles and code of conduct on AI aims to promote safe, secure and trustworthy AI (5). The White House Executive order on the Safe, Secure, and Trustworthy Development and Use of Artificial Intelligence follow similar principles and normatives for responsible use (6).
Recommendations for implementation and quality assurance of AI-based applications in radiotherapy were already published in 2020, but since new solutions are emerging, as well as new consistent data from the studies and clinical practice, it is highly possible that an update will be made in time to come (7).
Emvisioning the future
Before taking a decision on how to use AI in radiotherapy, the potential users should become aware of these new solutions, get informed, and take into account ethical principles. A well-balanced approach can bring together the precision, consistency, and performance of the AI with human abilities like integration, adaptation, and creativity, improving patient care and cancer outcomes.
MVision AI is providing a complex set of quality solutions, based on the international guidelines and recommendations, on both clinical aspects and data protection. We are supporting clinicians to enhance their capabilities and become more efficient and more knowledgeable, while following the ethical principles of AI use in Radiation Oncology.
References
- Farhud DD, Zokaei S. Ethical Issues of Artificial Intelligence in Medicine and Healthcare. Iran J Public Health. 2021;50(11):i-v. doi:10.18502/ijph.v50i11.7600
- Lahmi L, Mamzer MF, Burgun A, Durdux C, Bibault JE. Ethical Aspects of Artificial Intelligence in Radiation Oncology. Semin Radiat Oncol. 2022;32(4):442-448. doi:10.1016/j.semradonc.2022.06.013
- Ethics and governance of artificial intelligence for health. https://www.who.int/publications/i/item/9789240029200. Accessed on 17 December 2023.
- EU AI Act: first regulation on artificial intelligence. https://www.europarl.europa.eu/news/en/headlines/society/20230601STO93804/eu-ai-act-first-regulation-on-artificial-intelligence. Accessed on 17 December 2023.
- Hiroshima Process International Code of Conduct for Advanced AI Systems. https://digital-strategy.ec.europa.eu/en/library/hiroshima-process-international-code-conduct-advanced-ai-systems
- Executive Order on the Safe, Secure, and Trustworthy Development and Use of Artificial Intelligence. https://www.whitehouse.gov/briefing-room/presidential-actions/2023/10/30/executive-order-on-the-safe-secure-and-trustworthy-development-and-use-of-artificial-intelligence/. Accessed on 17 December 2023.
- Vandewinckele L, Claessens M, Dinkla A, et al. Overview of artificial intelligence-based applications in radiotherapy: Recommendations for implementation and quality assurance. Radiother Oncol. 2020;153:55-66. doi:10.1016/j.radonc.2020.09.008