Cardiac diseases and cancers are leading causes of death [1]. Many cancer patients have preexistent cardiac impairment or have risk factors of developing it. On the other hand, survival after being diagnosed with cancer is increasing, so relatively more patients may develop long-term side effects.
Cardiac diseases and cancers are leading causes of death [1]. Many cancer patients have preexistent cardiac impairment or have risk factors of developing it. On the other hand, survival after being diagnosed with cancer is increasing, so relatively more patients may develop long-term side effects.
Avoiding to irradiate healthy tissues is not something new in radiotherapy, but technology improvements make possible a shift in approach. Anatomical organs are heterogeneous volumes, made of different tissues. Differences in cell metabolism and blood supply are related to distinct vulnerability to ionizing radiation. Long-term cardiac function impairment is a concern when irradiating thoracic malignancies, such as lung, esophagus, or left breast cancers. Dose-response relationships have been studied for heart substructures, but further evidence is still needed [2].
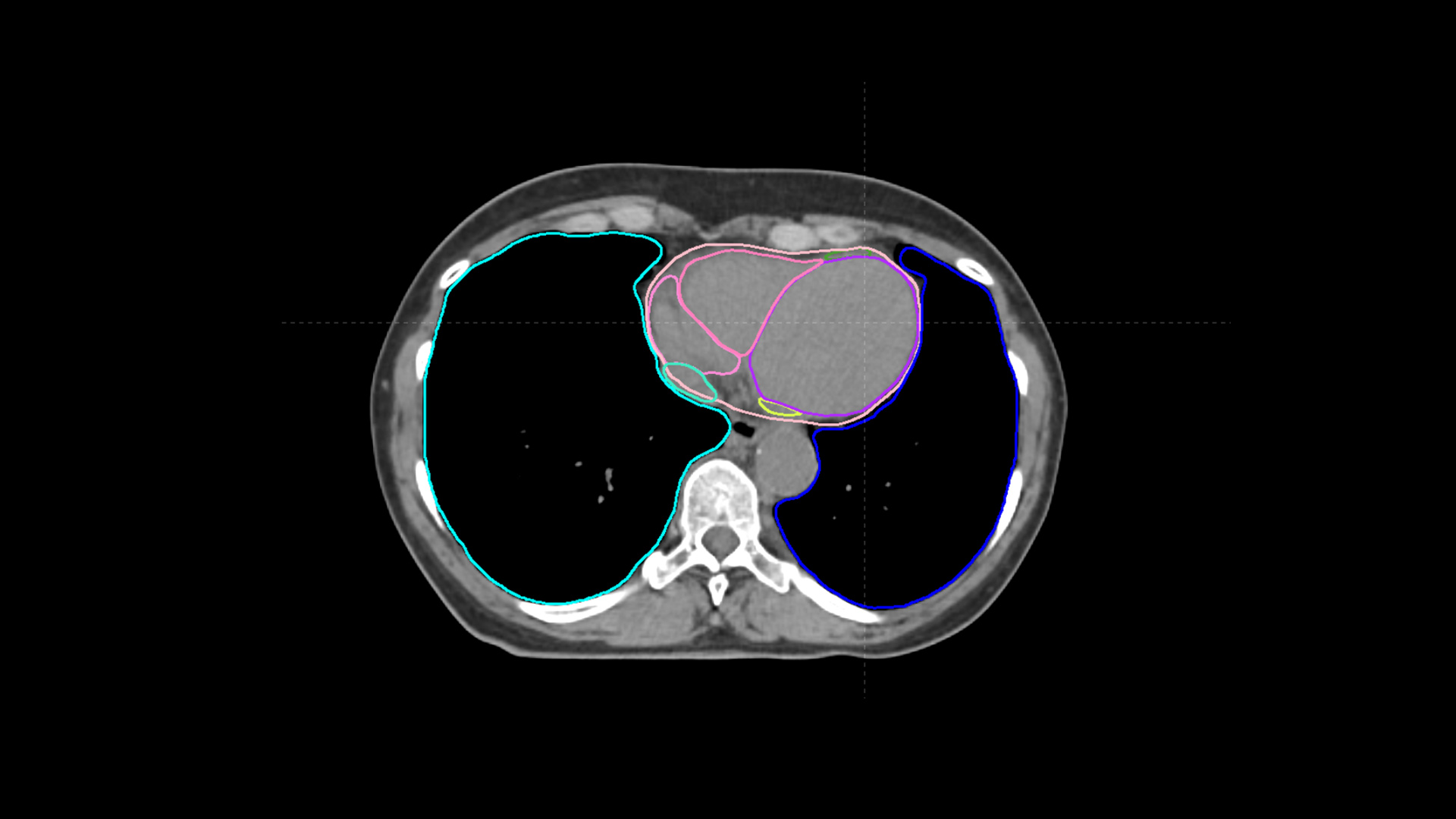
Analyzing correlations between the dose received by different substructures and toxicity, which can subsequently impact the non-cancer deaths, can identify the most vulnerable zones and new thresholds of safety. However, manual delineation of multiple structures would mean investing significant time resources from clinicians or researchers. In this context, AI-based solutions can contribute to advances in research. Auto-contouring of heart sub-structures by MVision AI Contour+ was successfully used by a team of Italian researchers from “Istituto Nazionale dei Tumori”, Milano. The results were presented at ESTRO 2024, first author being Alessandro Cicchetti [3].
The study analyzed cardiac survival-limiting toxicity and included data from 88 patients with non-resected locally advanced Non-Small Cell Lung Cancer patients treated with 50-66 Gy delivered by arc therapy. Nine cardiac substructures were automatically contoured: aorta, left anterior descending artery, pulmonary artery, left and right atrium, left and right ventricle, superior and inferior vena cava. For each structure mean dose and 2cc (D2cc) dose were calculated. Use of chemotherapy, dose to the lungs and the dose to the PTV were also included in the analysis. Then, a feature selection was applied to define the variables which are correlated to overall survival at 2 years follow-up.
D2cc to the aorta and left ventricle were associated with the survival-limiting toxicity, suggesting a different radiation response of heart substructures, like for a “serial type” organ, where impairing function of a segment impacts the segments which are connected, like in a chain. Also, the mean dose to the left lung was associated with overall survival, characteristic for “parallel type”, where damaging one part can be relatively compensated by the remaining functional parts.
Patients having high doses to all the three structures (aorta, left ventricle and lung) at the same time had a significantly higher risk of death (11 events over 15 patients). On the other hand, for the group of patients with low dose on the above-mentioned volumes, the death rate was much lower (3 events over 10 patients).
As underlined in the study’s conclusion, such models that include clinical risk factors and treatment data, including details about radiation therapy, could identify dose tolerance for the most radiosensitive anatomical heart substructures, improving the success rate of therapies, which are currently limited by adverse events. The dosimetric information can drive clinical practice toward a safe dose escalation protocol, taking advantage of the current technological level of the radiation therapy.
MVision AI Contour+ was created using advanced technology and aims to support Radiation Oncology professionals. Therefore, we are proud to further contribute to expanding knowledge through clinical research and improve cancer care.
References
[1] GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019 [published correction appears in Lancet. 2020 Nov 14;396(10262):1562]. Lancet. 2020;396(10258):1204-1222. doi:10.1016/S0140-6736(20)30925-9
[2] Banfill K, Giuliani M, Aznar M, et al. Cardiac Toxicity of Thoracic Radiotherapy: Existing Evidence and Future Directions. J Thorac Oncol. 2021;16(2):216-227. doi:10.1016/j.jtho.2020.11.002
[3] Cicchetti A et al. Cardiac Survival Limiting Toxicity in Locally Advanced Lung Cancer Patients Treated with RT.Radiotherapy and Oncology. Volume 194 Supplement 1, May 2024