The rate of new cases of cancer yearly is 442.4 per 100,000 amongst men and women per year (based on 2013–2017 cases). The most common cancers cases in 2020 were breast cancer, lung and bronchus cancer, prostate cancer, and colon and rectum cancer. Of the patients treated with cancer in America, 50% will receive radiation therapy during their course of illness. Furthermore, it is estimated that radiation therapy contributes around 40% towards curative treatment. (Baskar, Rajamanickam, et al.) This article will discuss the latest findings related to cancer care in radiotherapy in America, addressing geographical, financial, and telemedicine.

Geographical Access to Radiotherapy
As the ageing population in the US grows the cancer rates, cancer costs, and the need for geographically accessible radiotherapy treatment has grown too. “Radiation therapy is one of the primary treatments for cancer, but 1 in 20 Americans lives quite far from a radiation therapy clinic,” said lead author Sean Maroongroge, MD, MBA, a radiation oncology resident at The University of Texas MD Anderson Cancer Center. “If we do not incentivize or find ways to help people who live farther from treatment sites get access to radiation therapy, then this gap may continue to widen over time.”
According to a recent study presented at the 2020 American Society for Radiation Oncology (ASTRO) Annual Meeting, “The number of radiation therapy facilities in the United States has grown by 17% over the past 15 years.” (Maroongroge, S., et al.) Data for the study was collected from state regulatory agencies and national dosimetry monitoring organizations active between 2018 -2020. According to the ASCO Post, the researchers estimated that roughly 70% of the U.S. population lives within 12.5 miles of a treatment facility, and 4.5% of the population lives more than 50 miles from the closest radiation therapy facility.
“I have patients who just say that it’s just not feasible for them to get radiation if they have to travel a long distance. The financial stress and the weight of logistical burdens can’t be understated in terms of how much they dominate patients’ lives,” said Dr. Maroongroge. The factors affecting these trends were not determined in the study. However, validating the results with additional datasets could help better us identify populations at risk. (The ASCO Post)

Financial Burden of Cancer Care
A study published during July 2021 in National Cancer Institute’s Cancer Trend Progress Report focused on the financial burden of cancer care in America found that “national costs for cancer care were estimated to be $190.2 billion in 2015 and $208.9 billion in 2020 (2020 U.S. dollars), an increase of 10 percent that is only due to the aging and growth of the U.S. population.” These cost estimates factored in cancer-attributable costs for medical services. The highest medical services costs were for female breast, colorectal, lung, and prostate cancers and non-Hodgkin lymphomas. The cost estimates also factored in oral prescription drug costs. The highest oral prescription cost was found in female breast, leukemia, lung, and prostate cancers. The study also found that annualized average costs varied by stage in all phases of care.

Radiotherapy and Telemedicine
In October 2021, the JNCCN-National Comprehensive Cancer Network Journal, published a study evaluating patients’ satisfaction and preferences for telemedicine. Researchers reviewed survey responses from 1,077 radiation tumor patients worldwide. The questionnaire was based on office and telemedicine visits over the last 2 years.
Key findings included noteworthy information that “most people reported no difference or improvement in telemedicine overall compared to visits, confidence in physicians, and understanding of treatment plans. Most patients found that their cancers are treated appropriately, and 45% of cancer patients preferred telemedicine. Additionally, researchers have found that patient responses differ significantly between video conferencing and audio. Patients who booked by phone only tended to think that they would benefit more from a direct visit.”
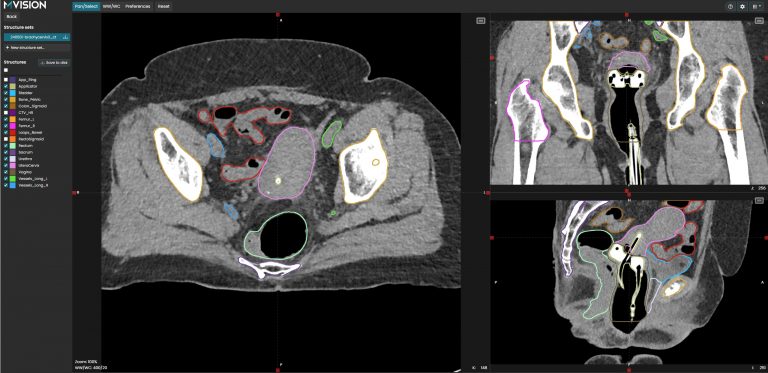
Guideline-based AI Segmentation, GBAIS™, radiotherapy software is coming soon to your American clinics
MVision AI is the pioneer of guideline-based AI segmentation, GBAIS™, radiotherapy software. We look forward to using our deep learning system to help you automate organ-at-risk contouring, including lymph nodes, to streamline your cancer treatment planning, as we are pending 510(k) FDA clearance. Robust HIPAA, and GDPR compliant, we bring the highest quality radiotherapy planning SaaS solution for your oncology department.
MVision AI is active on LinkedIn, Twitter, Facebook, and Instagram. Follow us on social media to stay up-to-date on the latest MVision AI news.
Are you eager to learn more? We welcome you to contact MVision AI:
c/o Terkko Health Hub, Haartmaninkatu 4, 00290 Helsinki, Finland.
Tel: +358 (0) 40 5489 229
Email: info (at) mvision.ai
For media inquiries:
+358 40 500 7915; pr (at) mvision.ai
Sources
Baskar, Rajamanickam, et al. “Cancer and Radiation Therapy: Current Advances and Future Directions.” International Journal of Medical Sciences, vol. 9, no. 3, 2012, pp. 193–199., https://doi.org/10.7150/ijms.3635.
“Cancer Statistics.” National Cancer Institute, https://www.cancer.gov/about-cancer/understanding/statistics.
“Financial Burden of Cancer Care.” Financial Burden of Cancer Care, National Cancer Institute, https://progressreport.cancer.gov/after/economic_burden.
“Geographic Access to Radiotherapy Facilities in the United States.” The ASCO Post, https://ascopost.com/news/october-2020/geographic-access-to-radiotherapy-facilities-in-the-united-states/.
Jameskusatsu. “JNCCN: Many Cancer Patients Receiving Radiation Therapy Prefer Telemedicine to Direct Visits: State.” Pennsylvania News Today, 19 Oct. 2021, https://pennsylvanianewstoday.com/jnccn-many-cancer-patients-receiving-radiation-therapy-prefer-telemedicine-to-direct-visits-state/249717/.
Maroongroge, S., et al. “Geographic Access to Radiation Therapy in the United States.” International Journal of Radiation Oncology*Biology*Physics, vol. 108, no. 3, 2020, https://doi.org/10.1016/j.ijrobp.2020.07.2270.